The Glasgow Coma Scale (GCS) was developed by Graham Teasdale and Bryan Jennett, neurosurgeons at the University of Glasgow, Scotland, in 1974. They designed the scale as a standardized method to assess and communicate the level of consciousness in patients with traumatic brain injuries (TBIs).
Teasdale and Jennett recognized the need for a simple and reliable tool that could be used by healthcare professionals across different settings to evaluate a patient's neurological status. They aimed to create a system that could provide a common language for describing levels of consciousness and facilitate communication among healthcare providers.
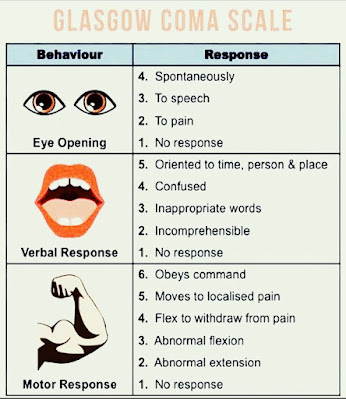
The GCS was based on observations and analysis of patients admitted to the neurosurgical unit at the Southern General Hospital in Glasgow. Teasdale and Jennett identified three key components of neurological function—eye-opening response, verbal response, and motor response—and assigned scores to each category based on the observed range of responses.
Their work resulted in the development of the GCS, which quickly gained acceptance and became widely used not only in the field of neurosurgery but also in emergency medicine, intensive care, and other healthcare specialties worldwide. The GCS has undergone revisions and refinements over the years to enhance its clinical utility, but the fundamental principles and scoring system established by Teasdale and Jennett remain the foundation of the scale.
ooo
EMS providers should have a good understanding of the Glasgow Coma Scale (GCS) as it is a vital tool for assessing a patient's level of consciousness. Here are a few key points about the GCS:
1. The GCS assesses three aspects of neurological function: eye-opening response, verbal response, and motor response. Each of these aspects is assigned a score ranging from 1 to 4 or 5, depending on the specific category.
2. The scores from each category are added together to give a total GCS score, which can range from 3 (indicating deep unconsciousness) to 15 (indicating full consciousness).
3. The GCS is commonly used to assess patients with TBIs or altered mental status. It provides a standardized and objective way to assess the severity of neurological impairment and monitor changes over time.
4. EMS providers should be familiar with the criteria for assigning scores in each category. For example, eye-opening response ranges from spontaneous (4) to no response (1), verbal response ranges from oriented conversation (5) to no verbal response (1), and motor response ranges from following commands (6) to no motor response (1).
5. The GCS score can help guide treatment decisions, determine the need for immediate intervention, and provide a baseline for assessing the patient's progress. Lower GCS scores generally indicate more severe neurological injury or impairment.
Remember, the GCS is just one tool among many that EMS providers utilize to assess and manage patients. It's important to consider other factors and clinical findings in conjunction with the GCS score to make informed decisions about patient care.
#EMS #GlasgowComaScale #PreHospitalCare #TraumaAssessment
No comments:
Post a Comment